By Miles Snowden, MD, Chief Medical Officer
In choosing hospital and facility-based medicine, we have chosen to be responsible for the highest acuity of healthcare needs. More often than not, for patients and families, high-acuity care is delivered by unfamiliar clinicians at unexpected times and in foreign facilities. Practicing this type of medicine well—one patient at a time—is remarkably difficult. Practicing this type of medicine well for an entire community affected by a high-impact event is a noble challenge indeed.
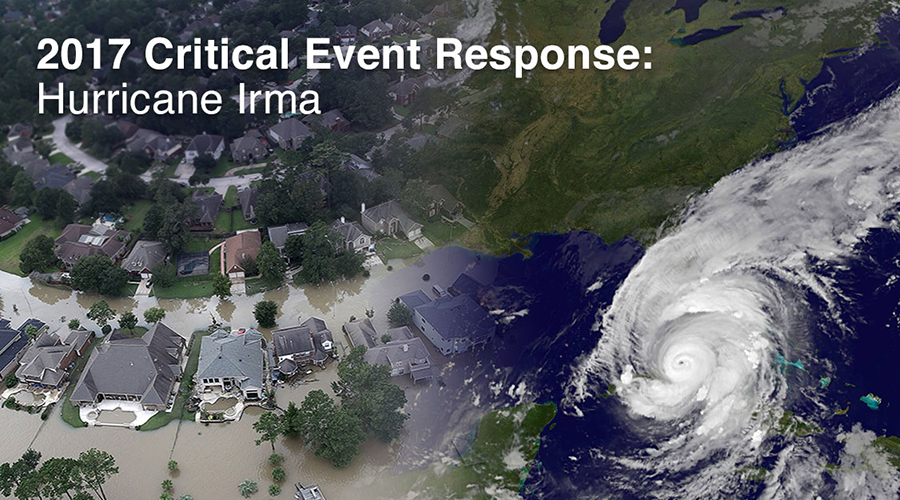
In 2017, TeamHealth responded to such community challenges several times. Our teams responded to Hurricane Harvey in Houston; Hurricane Irma in Florida; the tragic mass shooting in Las Vegas; the Atlas Peak wildfire in northern California; and Hurricane Maria in Puerto Rico.
Today, with our ever-larger footprint, it is increasingly likely that any U.S. natural disaster or mass casualty event will involve one of our TeamHealth communities. Are you ready?
What have we learned from our response to these 2017 events? How do we assure we are each ready when our turn comes? What does it take to respond to an extraordinary community critical event with extraordinary medicine?
During the 2018 National Medical Leadership Conference (NMLC), TeamHealth clinical leaders heard firsthand what it takes to respond to an extraordinary community event with extraordinary medicine. We learned from the experiences of three teams as they recounted how they responded to critical events in their communities.
In September 2017, Hurricane Irma, a powerful and catastrophic storm, made landfall in Florida after striking the Leeward Islands as a category five storm. At Marco Island, Irma made landfall as a category three storm with 120 miles-per-hour winds, which caused widespread power outages, flooding and significant damage. TeamHealth teams partnered with client facilities in the area to serve patients and families before, during and after the storm. This is the story of the firsthand experiences and best practices that arose from two healthcare facilities.
During NMLC, Dr. Steve Schwartz, President, Southeast Group, led a panel discussion regarding Hurricane Irma and the best practices learned from this critical event. Matt Stapleton, EVP, Anesthesiology, Dr. Jose Fernandez, Hospitalist Services Regional Medical Director (RMD) for Memorial Healthcare System, and Dr. Jeffrey Panozzo, Emergency Medicine FMD for North Naples Hospital, shared best practices learned from Hurricane Irma.
- Establish a remote incident command center where every service line is represented.
- Know that solutions may vary depending on event timing and location.
- Managing reassurance, support, resources and communication leads to better outcomes.
- Safety of family, loved ones and pets affect clinicians’ willingness to stay during a critical event.
- Expect the unexpected.
My hope is that these resources help all of us be better prepared for such events when our time comes.
It is also important to recall that many of our colleagues were personally, not only professionally, impacted by these critical events. Many colleagues lost utilities, autos, homes and other personal property. It is just as important we plan for the personal impact as the professional challenges of disaster and mass casualty events. After all, we can’t take care of others without also taking care of our own.
Thank you to all our clinical and non-clinical teams and your ability to lead and provide care in the most trying of times.
To learn more about a team that supports you and will be there for you on your best and worst days, connect with us. We care about you—clinicians who care for patients—and aim to provide resources you need, both professionally and personally.